The word ‘psychosis’ refers to a range of experiences or symptoms that can occur for someone. During experiences of psychosis, a person’s beliefs, thoughts, feelings, senses and behaviours can be affected. Psychosis can make it difficult to know what is real, and it is easy to misinterpret or confuse what is happening around you.
Most people at some stage in their life will experience challenges with their mental health and wellbeing, such as depression and anxiety. Similarly, experiences of psychosis can happen to anyone, regardless of their age, gender, culture or socioeconomic status.
Psychosis is common, and around 3 in 100 people will experience psychosis at some stage in their life. Most commonly psychosis can develop in people’s late teens and early twenties, which is why Early Intervention in Psychosis Services often work with young people, so they can support them the first time they start to experience psychosis.
Psychosis looks different for different people, and symptoms can change over time. Some common symptoms can include:
-
Having mixed up thoughts or finding it hard to think
-
Losing interest in hanging out, doing stuff and taking care of yourself
-
Hearing voices or sounds that others can’t hear (often called ‘hallucinations’)
-
Seeing things that aren’t there for others to see (also called ‘hallucinations’)
-
Having thoughts or ideas that don’t fit in with the reality they live in, and other people do not share or may think are strange (sometimes called ‘delusions’)
-
Thinking someone wants to harm them or their family
Psychosis often occurs in ‘episodes’, i.e. periods of time in which someone may experience quite intense symptoms, and which can have a big impact on life during that time. Click here to find out more about first episode psychosis.
There are treatments available for psychosis, including medication, talking therapies and social support. The earlier that someone receives treatment for psychosis the better. This is called Early Intervention (EIP), click here to find out more.
Interventions can help people to get through an episode and back into life again. Sometimes people may experience ongoing symptoms of psychosis, even once they are through an episode. However, people often find new ways of coping with these experiences so that they can continue living the life they want, rather than feeling held back by them.
If you are concerned that you or someone you care about may be experiencing signs of psychosis then you can find out about local Early Intervention Services here. You can also find out more about our ‘Something’s not quite right’ prompt sheet here which can be helpful to see what signs or symptoms of psychosis you or a family member might be experiencing.
If you or a family member are being supported by an Early Intervention Team then they will often provide information and education about psychosis. For further information about psychosis please click here for a range of useful websites and resources for people experiencing psychosis and their family members and friends.
Understanding psychosis experiences
We work with young people to look at what may have contributed to them developing experiences of psychosis, which can then help us to plan together what support is needed to help promote recovery and wellbeing and reduce the risk of a further episodes occurring (often called a relapse). For some people it can take some time to be able to recognise their experiences as symptoms of psychosis, because they can feel so very real. So EI teams may provide information about psychosis very gently and slowly, trying to meet the person where they are at.
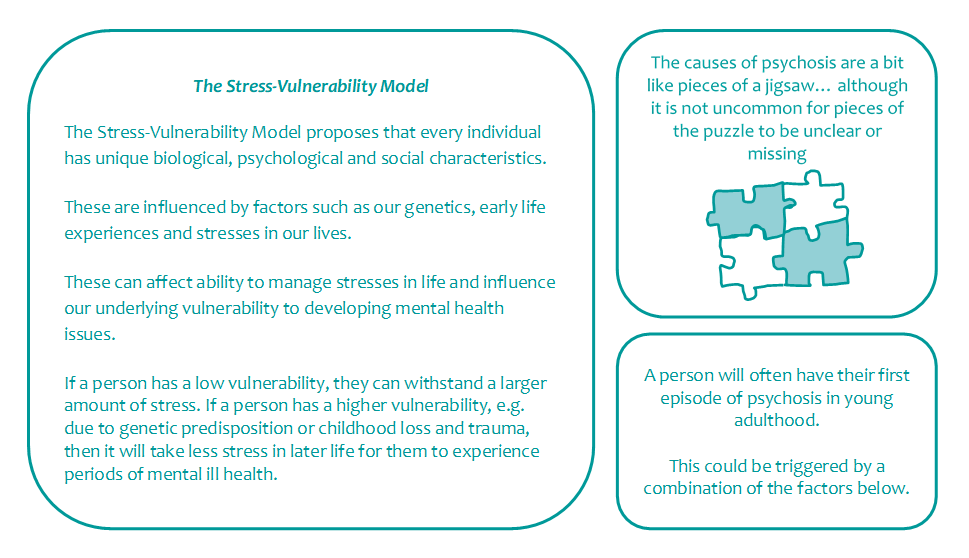
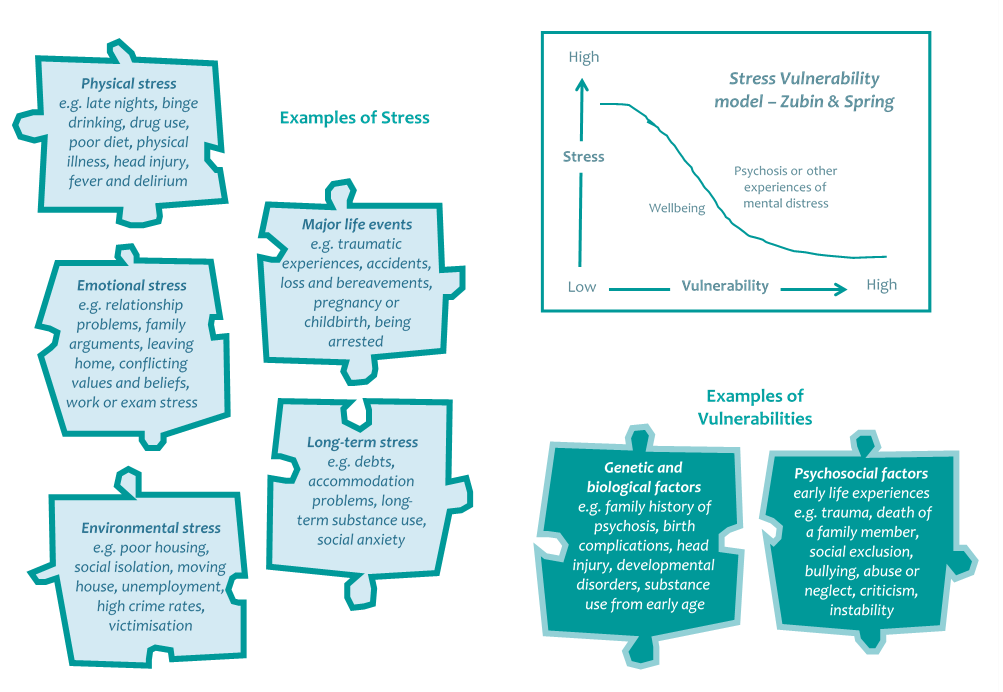
There is not just one, but a number of complex reasons why people develop psychosis. Some people may be more prone to developing psychotic symptoms under certain conditions than others. Although there are several factors that have been shown to increase someone’s risk of developing psychosis, we don’t always know why some people develop psychosis and others don’t. One way we try to understand why people may have developed psychosis by using the ‘Stress-Vulnerability’ Model, developed by Zubin and Spring back in 1977.
Understanding Māori experiences
For some Māori clients these experiences can be understood in the context of Matakite or Wairua experiences. You can read more about Matakite and Wairua experiences here.
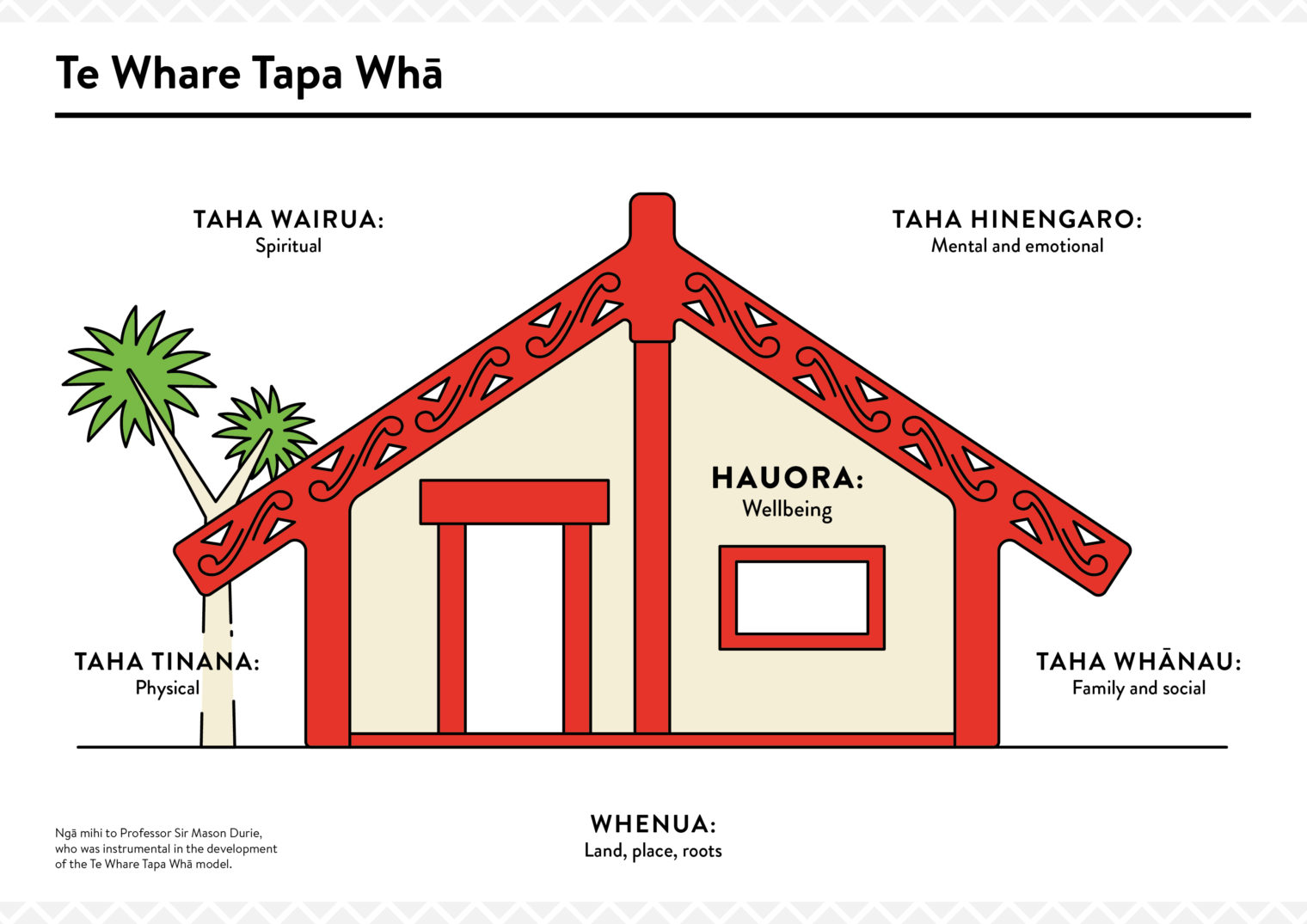
Another model that is commonly used in NZ is a model of Māori health and wellbeing called Te Whare Tapa Whā, developed by Sir Mason Durie in 1984. This can be another really useful way of helping young people and their whānau to understand why someone may be experiencing ill health.
The model suggests that health and wellbeing are like a wharenui/meeting house with four walls.
-
Taha wairua/spiritual wellbeing
-
Taha hinengaro/mental and emotional wellbeing
-
Taha tinana/physical wellbeing
-
Taha whānau/family and social wellbeing
Good health and wellbeing can be achieved when these different components are strengthened and we are connected to them; when there are challenges in one or more of these areas then we can become unbalanced in our life and experience distress or difficulty. You can find out more about the model here.